| Medical Finals contents: Welcome Finals advice Written exams Clinical revision X-Rays Mock final OSCE's |  |
Medical Finals contents: Monthly quiz PDA's Links Credits Your comments Who are we? |
MCQ's in Neurology |
Contributor: Dr. Ann Johnston Neurology SpR University Hospital of Wales Cardiff January 2006 |

|
Click on the radio-button to the left of the best answer from each of the five possible answers.
A tick mark ![]() will appear if you are right.
will appear if you are right.
A cross mark ![]() will appear if you are wrong.
will appear if you are wrong.
The correct answer will appear in the text-box area below each question.
Your score is updated near the bottom of this page. Only your first answer for each question counts towards your score.
However if your browser does not have javascript, then all the answers along with discussions are at the bottom of this page.
A young farmer presented with these acutely painful lesions on his lower legs.
 Not long afterwards his friends noticed he had an unusual facial appearance. In that he could not smile, close his left eye or wrinkle his forehead on the left. |
| 1.1: What are the painful lesions on his lower legs? |
| (a) Erythema multiforme | ||
| (b) Chronic plaque psoriasis | ||
| (c) Necrobiosis Diabeticorum | ||
| (d) Erythema marginatum | ||
| (e) Erythema nodosum |
| 1.2: What is the most likely diagnosis? |
| (a) Lyme disease | ||
| (b) Sarcoidosis | ||
| (c) Diabetes | ||
| (d) Guillian Barre Syndrome | ||
| (e) Bells palsy |
A slighty overweight lady has the following fundal appearance.
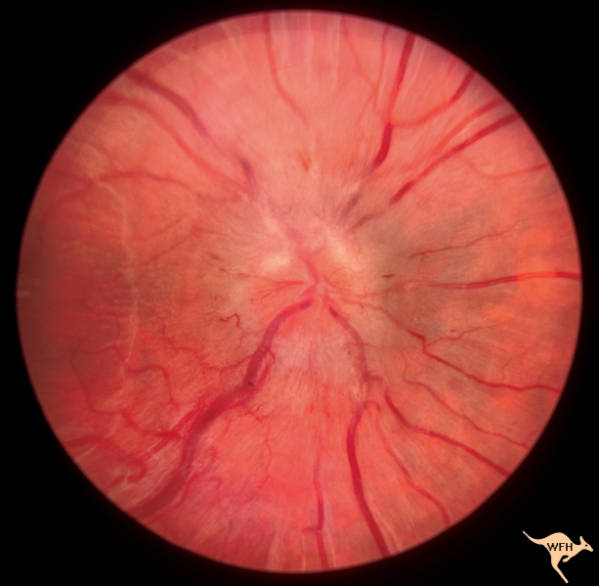 [Photo from: William F. Hoyt Neuro-Ophthalmology Collection] You also notice that she has a VIth nerve palsy. |
| 2.1: How would you describe the above appearance? |
| (a) Normal fundus | ||
| (b) Optic atrophy | ||
| (c) Papilloedema | ||
| (d) Retinitis pigmentosa | ||
| (e) Foster-Kennedy Syndrome |
| 2.2: Which one of the following tests would you most like to perform? |
| (a) Visual field testing | ||
| (b) Visual acuity | ||
| (c) Lumbar puncture | ||
| (d) CT scan | ||
| (e) Colour vision with Ishara plates |
| 2.3: All of the above investigations are subsequently performed. Brain imaging does not reveal any abnormality. What is the most likely diagnosis? |
| (a) Glioma | ||
| (b) Meningioma | ||
| (c) Pituitary adenoma | ||
| (d) Cortical venous sinus thrombosis | ||
| (e) Benign intracranial hypertension |
|
A 79 year old man presents with a gradual deterioration in mental state, he also has had difficulty in walking and has had frequent falls.
Here is his CT scan: 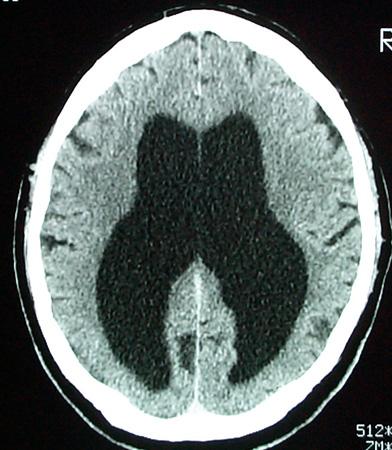 |
| 3.1: With this scan appearance, what other piece of clinical information will help to establish the diagnosis? |
| (a) Urinary incontinence | ||
| (b) Sexually inappropriate | ||
| (c) Auditory hallucinations | ||
| (d) Resting tremor | ||
| (e) Myoclonus |
| 3.2: What is the diagnosis? |
| (a) Alzheimers disease | ||
| (b) Parkinsons Disease | ||
| (c) Sporadic CJD | ||
| (d) Normal Pressure Hydrocephalus | ||
| (e) Multi-infarct dementia |
|
A 45 year old lady presents after a 6 week history of a painful neck. The pain is described as shooting in nature and 10/10 on a severity score. Now she describes a 3 day history of right arm weakness.
Examination reveals weakness on right shoulder abduction (4/5) and right elbow flexion (4/5). Reflexes in her right arm are all absent apart from triceps. There are no sensory findings. The remainder of the examination is normal. |
| What is the most likely diagnosis? |
| (a) CVA | ||
| (b) Cervical myelopathy | ||
| (c) Brachial neuritis | ||
| (d) Radial nerve palsy | ||
| (e) Frozen shoulder |
 |
|
Which of following could not be the diagnosis here? |
| (a) Left IIIrd nerve palsy | ||
| (b) Myasthenia gravis | ||
| (c) Horners syndrome | ||
| (d) Left VIth nerve palsy | ||
| (e) Lambert-Eaton Syndrome |
| A 66 year old man attends his GP with a troublesome tremor that has been present for about 10 years. It is present at rest, though becomes exaggerated with finger-nose testing. It is bilateral and occasionally you notice a no-no head tremor. On questioning he states that his father suffered from Parkinson's disease and he is concerned that he may now also have developed the condition. |
| 6.1: Which one of the following tests or investigations may be most helpful in diagnosing benign essential tremor from Parkinson's disease? |
| (a) CT brain | ||
| (b) Smell testing | ||
| (c) Glabellar tap | ||
| (d) Ease in amplitude of tremor with alcohol | ||
| (e) Trial of Madopar |
| 6.2: His past medical history includes asthma, COPD and stable angina. You accordingly ask him for a list of his medication. Which one of the following drugs concerns you regarding his current condition? |
| (a) Aspirin | ||
| (b) Simvastatin | ||
| (c) Salmeterol | ||
| (d) Carbamazepine | ||
| (e) Salbutamol |
| 6.3: He will not leave the consultation until you prescribe some medication for his current condition. Which of the following drugs is most appropriate? |
| (a) Madopar | ||
| (b) Sinemet | ||
| (c) Propanolol | ||
| (d) Gabapentin | ||
| (e) Atenolol |
A patient with normal IQ presents to the epilepsy clinic after several episodes of loss of consciousness and you notice these skin lesions.
 |
| 7.1: What are these skin lesions? |
| (a) Shagreen patchs | ||
| (b) Melanomas | ||
| (c) Café-au-lait spots | ||
| (d) Benign naevi | ||
| (e) Vitiligo |
| 7.2: You discover that his brother and father also have similar skin lesions. What is the diagnosis? |
| (a) Tuberous sclerosis | ||
| (b) Neurofibromatosis type I | ||
| (c) Neurofibromatosis type II | ||
| (d) Downs syndrome | ||
| (e) Hereditary haemorrhagic telangiectasia |
| 7.3: What or where is the chromosomal abnormality? |
| (a) Trisomy 21 | ||
| (b) Chromosome 22 | ||
| (c) Chromosome 17 | ||
| (d) Chromosome 11 | ||
| (e) CAG Triple repeat chr 4 |
| You examine a 78 year old right handed man who is dysphasic and the nurses tell you that he has suffered from a stroke. |
| 8.1: Which one of the following clinical signs would you expect to find? |
| (a) Left extensor plantar | ||
| (b) Left homonymous hemianopia | ||
| (c) Left sided hemiplegia | ||
| (d) Right homonymous hemianopia | ||
| (e) Right lower motor neurone VIIth nerve palsy. |
|
8.2: Afterwards you examine the gentleman in the next bed who is also right handed. Visual field testing demonstrates a lower left quadrantanopia. Where is the lesion causing this visual field defect? |
| (a) Right temporal lobe | ||
| (b) Right parietal lobe | ||
| (c) Left temporal lobe | ||
| (d) Right temporal lobe | ||
| (e) Optic chiasim |
| 8.3: In the same man, which of the following features may also be present? |
| (a) Agraphia | ||
| (b) Acalculia | ||
| (c) Left-Right disorientation | ||
| (d) Finger agnosia | ||
| (e) Constructional apraxia |
| 30 year old gym instructor, describes one episode of severe occipital headache while exercising vigorously in the gym. He also reports another similar episode of severe headache during sexual intercourse after which he vomited. No signs on examination. |
| 9.1: What is the most likely diagnosis? |
| (a) Subarachnoid haemorrhage | ||
| (b) Migraine | ||
| (c) Herald bleed | ||
| (d) Muscle tension headache | ||
| (e) Subdural haemorrhage |
| 9.2: What investigations are required? |
| (a) CT brain | ||
| (b) Lumbar puncture | ||
| (c) None | ||
| (d) CT angiogram | ||
| (e) Formal angiography |
| 9.3: What treatment is required? |
| (a) Nimodipine 4 hourly | ||
| (b) Aneurysm coiling | ||
| (c) Aneurysm clipping | ||
| (d) Burr hole surgery | ||
| (e) Beta-blockers |
| A 50 year old male presents with a lower motor neurone VIIth nerve palsy, his family are concerned that he has suffered a stroke. He has deafness in his right ear which he says is long-standing though has seen ENT who diagnosed this as sensorineural deafness. He now also complains of double vision on right lateral gaze with horizontal separation of the images. |
|
10.1: You examine his eyes, and find incomplete abduction of the right eye on right gaze. The rest of his eye movements are full. The pupils are equal and react appropriately to light and accommodation.
What do you diagnose? |
| (a) Right VIth nerve palsy | ||
| (b) Right IIIrd nerve palsy | ||
| (c) Right IVth nerve palsy | ||
| (d) Right Horners | ||
| (e) Right internuclear opthalmoplegia |
| 10.2: His corneal reflex is absent. Where do you place the pathology? |
| (a) Cavernous sinus | ||
| (b) Jugular foreman | ||
| (c) Midbrain | ||
| (d) Cerebellopontine angle | ||
| (e) Skull base |
PLEASE give us some feedback, using the comments form about what you think of the questions (relevance, level of difficulty, what you would like to see more of etc.), so that we can further update the site appropriately. Thankyou.
| 1.1 | (e) Erythema nodosum |
| 1.2 | (b) Sarcoidosis |
| 2.1 | (c) Papilloedema |
| 2.2 | (d) CT scan |
| 2.3 | (e) Benign intracranial hypertension |
| 3.1 | (a) Urinary incontinence |
| 3.2 | (d) Normal Pressure Hydrocephalus |
| 4 | (c) Brachial neuritis |
| 5 | (d) Left VIth nerve palsy |
| 6.1 | (b) Smell testing |
| 6.2 | (e) Salbutamol |
| 6.3 | (d) Gabapentin |
| 7.1 | (c) Café-au-lait spots |
| 7.2 | (b) Neurofibromatosis type I |
| 7.3 | (c) Chromosome 17 |
| 8.1 | (d) Right homonymous hemianopia |
| 8.2 | (b) Right parietal lobe |
| 8.3 | (e) Constructional apraxia |
| 9.1 | (b) Migraine |
| 9.2 | (c) None |
| 9.3 | (e) Beta-blockers |
| 10.1 | (a) Right VIth palsy |
| 10.2 | (d) Cerebellopontine angle |
Answers Case 1:1.1: (e) Erythema nodosum 1.2: (b) Sarcoidosis Discussion:This patient presents with painful red lesions on his shins together with a facial palsy. The facial appearance represents a VIIth nerve palsy, in this instance a lower motor neurone VIIth. The key to this question is linking conditions that cause a VIIth nerve palsy with painful skin lesions on the legs. Acute onset of painful red lesions on anterior shins is almost characteristic of erythema nodosum. Some causes of unilateral VIIth nerve palsy:
Some causes of erythema nodosum:
A few clinical features of sarcoidosis (Many - multi-system disorder!!):
|
Answers Case 2:2.1: (c) Papilloedema 2.2: (d) CT scan 2.3: (e) Benign intracranial hypertension Discussion:This case is classic for benign intracranial hypertension. It usually presents in young women with a raised BMI.The retinal photograph demonstrates raised intracranial pressure, as shown by the papilloedma, with evidence of a pink disc, blurred margins and haemorrhages. All of the mentioned investigations are appropriate here, though given the papilloedema, a space-occupying lesion must first be excluded. This is easily done with a CT scan. Though in clinical practice a CTV (CT venogram) may also be required to exclude the possibility of a venous sinus thrombosis. Benign intracranial hypertension, the brain imaging is normal in the vast majority. In some instances there may be slight venricular dilation. Note - that the VIth nerve palsy here is a false localising sign of raised intracranial pressure. Potential causes of benign intracranial hypertension:
|
Answers Case 3:3.1: (a) Urinary incontinence 3.2: (d) Normal Pressure Hydrocephalus Discussion:This case represents one of normal pressure hydrocephalus. Clinically described as a triad of - urinary incontinence, falls (gait apraxia) and dementia.CT scan or MRI will demonstrate ventricular dilation. This is a potentially treatable cause of dementia. The treatment option in the first instance is lumbar puncture. If a clinical improvement is shown with lumbar puncture then the patient may benefit from VP shunt. |
Answer Case 4:(c) Brachial neuritis Discussion:History is an acute onset, painful event affecting shoulder abduction (C5) and elbow flexion (C6). Examination demonstrates weakness in these myotomes and loss of biceps reflex (C5, C6) and supinator (C6), with sparing of triceps (C7). This is a fairly characteristic description of brachial neuritis. I would also expect the muscle brachioradialis (C6) also to be affected and therefore weak.A CVA, would cause upper motor neurone signs. Cervical myelopathy could cause this picture if the lesion was at C5-C6. Though upper motor neurone signs would be expected below the level of the lesion. Remember that a spinal cord lesion can cause lower motor neurone signs at the level of the lesion due to compression of nerve roots and upper motor neurone lesion below the level of the lesion. A radial nerve palsy, causes wrist drop resulting from weakness of wrist extensors, finger extensors, supinator and extensor carpi radialis. Classically occurs as a "Saturday night palsy" (patient falls asleep with arm hanging over back of chair), in which the nerve is compressed against middle third of humerus. Only if the nerve is compressed in the axilla, will weakness of triceps occur (C7) together with loss of the triceps reflex. A frozen shoulder causes stiffness and painful restriction of all shoulder movements, felt to be due to an adhesive capsulitis and responds to intra-articular steroids injections and physio. |
Answer Case 5:(d) Left VIth nerve palsy Discussion:This is the only option that does not cause ptosis! |
Answers Case 6:6.1: (b) Smell testing 6.2: (e) Salbutamol 6.3: (d) Gabapentin Discussion:This is a difficult case though a very common clinical scenario. This gentleman has benign essential tremor. Outlined by a tremor with a major action component and with head involvement. It is also bilateral.In contrast Parkinsons disease is initially an asymmetric condition, characterised by rest tremor, bradykinesia and rigidity. Many tremors can have action and resting components to them and they do not always fit the textbook description. Alcohol can relieve all tremors though it is classically said that it characteristically eases benign essential tremor. Recent research has demonstrated that sense of smell is lost in Parkinsons disease. On direct questioning patients deny this though it can be accurately tested for and be a good discriminating test in distinguishing benign tremor from Parkinsons disease. A DAT scan may be helpful in distinguishing the two conditions, as it outlines dopamine deplete areas. B2 agonists like Salbutamol can cause tremulousness as an unwanted side-effect. Treatment options usually are nothing or Beta-blockers. However Beta-blockers are contra-indicated here as this gentleman suffers from asthma and COPD! Other alternative options include, Gabapentin, Pregabalin, Topiramate and Levitaracetam. |
Answers Case 7:7.1: (c) Café-au-lait spots 7.2: (b) Neurofibromatosis type I 7.3: (c) Chromosome 17 Discussion:This case provides an opportunity to revise neurofibromatosis. The skin lesions associated with it and the absence of skin lesions in type II. (Chromosome 22). Type II presents with bilateral acoustic neuromas.Important to distinguish it from tuberous sclerosis, which will present with learning difficulties, decreased IQ and a different set of skin lesions. Tuberous sclerosis is also mainly autosomal dominant like neurofibromatosis. Epilepsy is common in both conditions and so knowledge of the skin lesions can often be helpful in obtaining a diagnosis. |
Answers Case 8:8.1: (d) Right homonymous hemianopia 8.2: (b) Right parietal lobe 8.3: (e) Constructional apraxia Discussion:The first man is right handed so left hemisphere dominant, with affected speech therefore the stroke has affected the left hemisphere involving speech centre in left temporal lobe.Clinical signs expected would be a right homonymous hemianopia, right upper motor neurone VIIth nerve palsy, right hemiplegia - with increased tone, reflexes and an extensor plantar on the right. The second man, is also right handed so therefore left hemisphere dominant. He has a left visual field defect, therefore right sided brain pathology in his parietal lobe. A temporal lobe lesion would give a superior quadrantanopia. As this gentleman has a lesion in his non-dominant parietal lobe, constructional or dressing apraxia may be seen. All the other features are dominant parietal lobe signs. |
Answer Case 9:9.1: (b) Migraine 9.2: (c) None 9.3: (e) Beta-blockers Discussion:Again a tricky case but a common clinical scenario and I am open to debate regarding the correct answers.The key to this case is the fact that this is not an isolated episode. It has happened previously with no neurological sequeli. However if this was his first episode he would of course warrant investigation for subarachnoid haemorrhage. Which would include a CT brain followed by a lumbar puncture if the CT scan was normal. Migraine associated with vigourous exercise and with sexual intercourse can be very disabling and does warrant treatment. Prophlaxis with Beta-blockers is generally recommended, despite the obvious side-effect of impotence!! |
Answer Case 10:10.1: (a) Right VIth palsy 10.2: (d) Cerebellopontine angle Discussion:This is a case of a cerebellopontine angle lesion. Which presents with senroineural deafness (therefore the underlying cause most likely to be an acoustic neuroma) - VIIIth, LMN VIIth, VIth nerve and Vth nerve palsies.The corneal reflex will be lost first. Other potential causes include a meningioma. |