| Medical Finals contents: Welcome Finals advice Written exams Clinical revision X-Rays Mock final OSCE's |  |
Medical Finals contents: Monthly quiz PDA's Links Credits Your comments Who are we? |
Question 1 | |||||
These are the fingers of a 25 year old man who suffers from a chronic disease. His FEV1 is 0.5 litres and his BMI is 18 kg/m2.
 What is the most likely diagnosis? | |||||
| |||||
|
Answer: (a) Cystic fibrosis
All of the options listed are possible causes of finger clubbing. The very poor lung function, as evidenced by the FEV1 of 0.5 litres, points to a respiratory condition. The low BMI, young age and chronicity of disease makes cystic fibrosis (CF) the most likely diagnosis. Nutritional deficiency in CF is caused by a combination of malabsorption and pancreatic insufficiency. Although Inflammatory Bowel Disease can result in low body weights in young people, respiratory function is not compromised. |
Question 2 | |||||
|
The same patient as in Question 1 develops acute abdominal pain with a serum amylase of 1784 iu/litre.
What is the most appropriate initial course of action? | |||||
| |||||
|
Answer: (b) Nil by mouth & IV fluids
Patients with cystic fibrosis have an increased risk of pancreatitis. Interestingly, it usually occurs in those who are pancreatic sufficient. The clinical course is usually not as severe as pancreatitis caused by alcohol or gallstones. As with any cause of pancreatitis the initial course of action is conservative management with ‘nil by mouth’ and IV fluids. If the patient becomes increasingly unwell in terms of worsening white cell count, lactate dehydrogenase, urea, arterial oxygen levels, serum calcium, glucose, or urine output then they may need surgery or intensive care treatment. IV antibiotics may be required. The severity of acute pancreatitis is scored using either the Ranson or Glasgow criteria. Measurements are made within 48 hours of presentation, with 3 or more positive factors indicating severe pancreatitis which correlates with an increased mortality rate. |
Question 3 | |||||
| In the same patient, colonisation with which of the following organisms is associated with the poorest prognosis? | |||||
| |||||
|
Answer: (a) Burkholderia Cepacia
Streptococcus pneumoniae and Haemophilus influenzae are involved in community acquired infections, not just in patients with CF. They tend to be responsible for acute exacerbations and are usually sensitive to penicillin antibiotics. Burholderia cepacia is a very resistant organism and chronic colonisation in patients with CF causes gradual but progressive decline in lung function. There is no evidence that MRSA carries a worse prognosis. Colonisation with Pseudomonas aeruginosa is common in patients with CF and bronchiectasis, and although it does cause decline in lung function, in the long term it is a more sensitive organism than Burkholeria cepacia. |
Question 4 | |||||
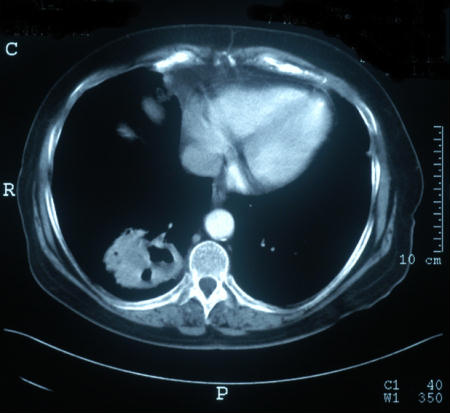
This is a CT scan of the chest of a 49 year old lady with haemoptysis. She is a life-long smoker. She is apyrexic. Her CRP and ESR are normal, and her PaO2 is 9.5 kPa.
 What is the most likely diagnosis? | |||||
| |||||
|
Answer: (d) Lung Cancer
The CT film shows a cavitating lung lesion in the right lower lobe. Causes of cavitating lung lesions:
This patient is apyrexic with normal inflammatory markers making infection or abscess less likely. ESR would usually be elevated in Wegener’s granulomatosis, and the history is not consistent with COPD. The history of smoking lends further weight to an underlying malignancy. |
Question 5 | |||||
This is the same patient undergoing a CT guided biopsy.
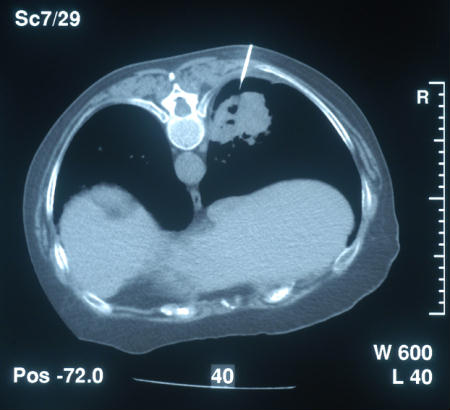 Which of the following investigations is it essential to check before performing this procedure? | |||||
| |||||
|
Answer: (a) Coagulation screen
To reduce the risk of haematoma or haemothorax formation, it is essential to check the coagulation profile. |