| Medical Finals contents: Welcome Finals advice Written exams Clinical revision X-Rays Mock final OSCE's |  |
Medical Finals contents: Monthly quiz PDA's Links Credits Your comments Who are we? |
Question 1 | |||||
|
A 21 year old female who is 26 weeks pregnant is admitted with 3 generalised tonic clonic seizures. She has no previous history of epilepsy. Her blood pressure is noted to be 210/90. Temperature is 37.9 °C. Urinalysis demonstrates marked proteinuria.
What is the ultimate management of this patient? | |||||
| |||||
|
Answer: (d) Deliver fetus and placenta
This lady has pre-eclampsia until proven otherwise. As outlined by: seizures, hypertension and proteinuria. Ultimately this can only be managed by inducing labour and delivering the fetus and the placenta. This is an emergency and other treatments only delay problems. The fetus must be delivered. |
Question 2 | |||||
The following picture shows the blue-gray skin discoloration which can be a side-effect of amiodarone:
(Picture from: American Family Physician - Photo) The following are also known side-effects of Amiodarone EXCEPT for one: | |||||
| |||||
|
Answer: (d) Pancreatitis
Amiodarone is a powerful, effective antiarrhythmic. However long-term use can cause significant toxicity. Organs that can be affected include: (i) Thyroid - as shown in the follwoing chemical structure, amiodarone contains iodine - remember the "iod" in the middle or Am-iod-arone:
 (Image from: rxlist.com) Hence can cause; - Hyperthyrodism - 2 types: due iodine overload, or due to acute thyroiditis - Hypothyrodism. (ii) Heart - Bradycardia, conduction disturbances, hypotension. (iii) Lungs - Pulmonary alveolitis, pneumonitis, and fibrosis. (iv) Liver - jaundice, hepatitis, cirrhosis. (v) Skin - slate-gray discoloration - which is persistent but quite rare. (vi) Nerves - Peripheral neuropathy and myopathy. (vii) Avoid in pregnancy & breast feeding. (viii) Other - impaired vision, haemolytic anaemia, GI disturbances, interaction with other drugs (eg. warfarin, digoxin, other anti-arrhythmics). Amiodarone can help suppresses life-threatening ventricular arrhythmias. It is currently the recommended drug for treating refractory VF/VT in the acute resusitation situation, where 300mg of amiodarone is made up in 20ml 5% dextrose is given as an intravenous bolus. However as it prolongs the QTc interval, it is best avoided where QTc is already prolonged. (For more details see: www.Anaesthetist.Com - Amiodarone ) |
Question 3 | |||||
| Which of the following conditions is paired incorrectly with the corresponding gait disturbance? | |||||
| |||||
|
Answer: (b) C5/C6 myelopathy - high stepping gait
Cervical myelopathy = spastic gait. A high stepping gait would be caused by foot drop (an inability to dorsiflex the foot). Sometimes a sensory deficit will cause a sensory ataxia and a slapping foot type gait. |
Question 4 | |||||
|
A 66 year-old man with bony pain undergoes a radioisotope bone scan. He is found to have multiple osseous metastases in the axial skeleton. The primary, at the time, has not been identified.
Which of the following tumours typically causes osteosclerotic metastases? | |||||
| |||||
|
Answer: (d) Prostate
Osseous (bony) metastases can be either osteolytic (destructive) or osteosclerotic (forming) in nature. The majority of osseous metastases are osteolytic and these destructive areas are seen as lucent ('darker') areas on plain x-rays. Osteosclerotic metastases are seen as sclerotic ('whiter') areas. Osteosclerotic metastases are characterized by increased new bone formation due to osteoblastic activity. The commonest causes are primary prostate and breast malignancies. Due to the increased turnover within these lesions they can be clearly seen on a radioisotope bone scan (a nuclear imaging technique). Metastatic lesions are observed as areas of increased uptake ('hot spots'). |
Question 5 | |||||
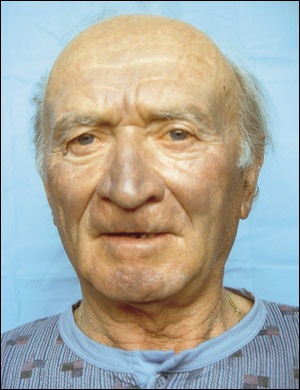
This gentleman presented with this facial appearance and had altered sensation on his left forehead.
 Which of the following could not cause this appearance? | |||||
| |||||
|
Answer: (e) Congential Horner's
This patient has Horner's syndrome which can be caused by any of the mentioned causes. Anything that interrupts the sympathetic chain as it passes from its beginning in the brainstem to the orbit may cause Horner's syndrome. However, it could not be congential, as a congential Horner's invariably has heterochromia! (Two different coloured eyes). |