| Medical Finals contents: Welcome Finals advice Written exams Clinical revision X-Rays Mock final OSCE's |  |
Medical Finals contents: Monthly quiz PDA's Links Credits Your comments Who are we? |
Question 1 | |||||
|
A 75 year old gentleman is admitted via ambulance to A & E. He gives a 4 hour history of vague upper abdominal discomfort. There is no radiation. He also complains of feeling dizzy.
Relevant past medical history includes: an abdominal aortic aneurysm repair/stenting performed 3 months previously via percutaneous technique. He tells you he was admitted 2 weeks ago for 2 days of observation as follow up ultrasound scan had revealed a small leak at the site of repair. He has never been treated for ischaemic heart disease. On examination he is fully conscious and alert. Heart rate is 70bpm regular and BP is 110/68. Heart sounds one and two are present and normal in character. There are no additional heart sounds or murmurs. Auscultation of the chest is clear. His left femoral pulse is very difficult to palpate. You perform an ECG: 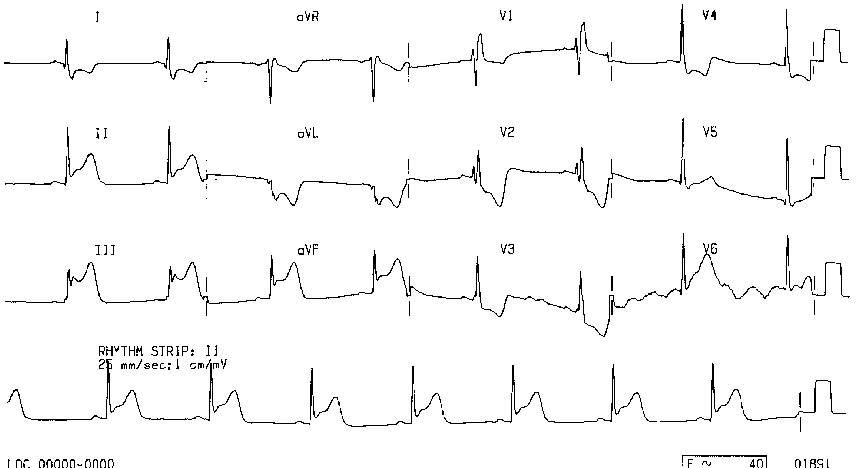
ECG image from: ecglibrary.com What is the diagnosis? | |||||
| |||||
|
Answer: (d) Infero-posterior myocardial infarction
The ECG is in sinus rhythm. There is ST segment elevation in the inferior leads (II, III and aVF), with marked reciprocal ST segment depression in leads V2 and V3. |
Question 2 | |||||
| What is your initial management of the above patient? | |||||
| |||||
|
Answer: (c) Aspirin 300mg, clopidrogrel 300mg, enoxaparin 60mg, metoprolol 5mg IV, transfer for primary angioplasty and stenting
The patient has recently had a major vascular procedure performed, and therefore thrombolysis with reteplase is contra-indicated. The patient should be transferred to the cardiac catheterization laboratory for primary angioplasty. |
Question 3 | |||||
| Which coronary artery do you think is affected in the above patient? | |||||
| |||||
|
Answer: (c) The right coronary artery (RCA)
This is usually the culprit artery in infarcts of this type. |
Question 4 | |||||
During transfer to the ward he suddenly loses consciousness. You immediately note the ECG defibrillator/monitor rhythm has changed. (see below)
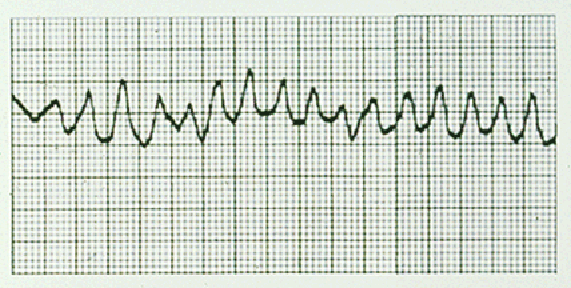
ECG image from: images.emedicinehealth.com What is your immediate treatment? | |||||
| |||||
|
Answer: (d) Administer 200 J DC biphasic shock
The rhythm strip shows ventricular fibrillation (VF). The most effective treatment for this is a DC shock. The most recent advanced life support guidelines (Resuscitation Council UK) would suggest that a 150-200 J shock from a biphasic defibrillator would be most appropriate. Quoting from section 5 of the current (2005) in-hospital resuscitation guidelines: "5. If the patient has a monitored and witnessed cardiac arrest: As this patient is already connected to a defibrillator/monitor, giving an immediate shock is best option. (Note: CPR at 15:2 is for Pediatrics, whereas 30:2 is used for adults.) |
Question 5 | |||||
Your treatment is successful and he regains consciousness. He is treated in the cardiology department, makes a successful recovery and is discharged. He returns 6 months later complaining of syncope. His ECG has changed again. (see below)
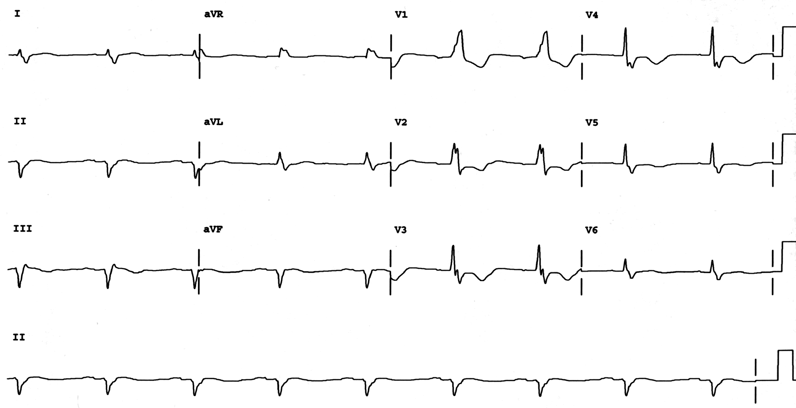
ECG image from: sprojects.mmi.mcgill.ca What is the diagnosis? | |||||
| |||||
|
Answer: (c) Old infero-posterior infarct, and trifascicular block
The presence of Q waves in the inferior leads with small R waves, and the presence of a dominant R wave in V1 suggests an old infero-posterior myocardial infarction. The presence of right bundle branch block, left axis deviation and first degree atrio-ventricular block indicates tri-fascicular block. |