| Medical Finals contents: Welcome Finals advice Written exams Clinical revision X-Rays Mock final OSCE's |  |
Medical Finals contents: Monthly quiz PDA's Links Credits Your comments Who are we? |
Question 1 | |||||
A 22 year old girl is brought to the emergency department after allegedly taking 30 x 500mg tablets of paracetamol. Her 4 hour post ingestion serum paracetamol levels are 136 mg/L.
 Which of the following conditions would place her in the high risk category and therefore require her to receive the N-acetyl cysteine antidote infusion? | |||||
| |||||
|
Answer: (c) Past history of anorexia nervosa with current BMI < 20.
The current low body mass with a previous history of an eating disorder places the patient into the high risk category of the paracetamol overdose nomogram. Paracetamol is a relatively safe drug at therapeutic levels. However if excessive amounts are taken (typically > 20x500mg) the liver stores of glutathione, essential for the safe metabolism of paracetamol, become rapidly depleted, producing an excess amount of the toxic paracetamol intermediary metabolite NABQI (N-acetyl-p-benzoquinoneimine). N-acetyl cysteine provides glutathione, allowing safe metabolism of this toxic intermediary. Any condition that predisposes to malnutrition or low liver stores of glutathione will result in a higher risk if a paracetamol overdose occurs. Examples of high risk cases are:
Concurrent overdose with codeine or benzodiazepines may complicate the supportive management of the patient but will not influence the decision to treat with N-acetyl cysteine. In an otherwise healthy individual with a normal diet, the hepatic glutathione stores will have been well replenished following the paracetamol overdose a year ago. Prolonged QT interval may occur in other poisonings such as tricyclics, sotalol and amiodarone. |
Question 2 | |||||
|
A 66 year old man with a 5 year history of hypertension was found to have a serum potassium level of 6.2 mmol/L on routine testing. This was confirmed on repeat testing.
Which of his other medications are most likely to have contributed to his hyperkalaemia? | |||||
| |||||
|
Answer: (d) Perindopril
Typical drugs that induce hyperkalaemia are:
Aspirin may sometimes cause thrombocytopenia, but has no effect on serum potassium. Bendroflumethazide as a thiazide may contribute to hypercalcaemia, hyperuricaemia and hyperglycaemia, but will lower serum potassium and sodium. Pravastatin as a HMG CoA reductase inhibitor (statin), may cause elevation of liver enzymes or of creatine kinase (CK) in susceptible individuals, but has no effect on serum potassium. |
Question 3 | |||||
A 64 year old man presented to the emergency department with a cough and shortness of breath. He was commenced on an unknown antibiotic and sent home. Three days later he attends his GP with increased skin pigmentation in the distribution shown.
 Which of the following antimicrobial treatments is the likely cause? | |||||
| |||||
|
Answer: (e) Levofloxacin
Photosensitive drug eruptions are adverse reactions of the skin that result from simultaneous exposure to a drug and to ultraviolet radiation or visible light. There are two types of photosensitive eruptions:
Phototoxic eruptions are most common. They usually occur on first exposure and do not recur when the drug is stopped except for those drugs having a long half-life. It is usually caused by ingested or injected drugs. The eruption may be immediate, with the appearance of erythema and edema, or delayed with an exaggerated sunburn pattern at 16-24 hours. Melanin hyperpigmentation and desquamation may follow. Stinging or burning of the skin often accompanies it. UV-A is most often responsible although UV-B and visible light may elicit this reaction with some drugs. Photoallergic eruptions are less common. They rarely occur on first exposure to the drug unless the patient was previously sensitized. It usually takes 7-10 days after the first exposure and 1-2 days after subsequent exposures for development. Topically applied drugs are the most frequent cause although systemically administered drugs may also be causative. Photoallergic reactions may be due to delayed hypersensitivity. The acute eruption may resemble urticaria, eczematous dermatitis, or a lichenoid papular eruption. The chronic phase of photoallergy shows scaling and lichenification with accompanying pruritus. Histologic examination reveals epidermal spongiosis, acanthosis, and a lymphocytic infiltrate. Photoallergic reactions may continue to recur on subsequent exposure to light without reapplication of the photosensitizer. Quinolones (except moxifloxacin) and tetracyclines are the most common classes of antimicrobials associated with photosensitive drug eruptions. Ceftazidime and cefuroxime may result in a photosensitive reaction but it is uncommon to cephalosporins and not described with cefaclor. Penicillins and macrolides (except azithromycin) are not usually associated with this kind of reaction. |
Question 4 | |||||
| Which of the following statements regarding anticoagulant therapy is correct? | |||||
| |||||
|
Answer: (a) The anticoagulant effect of warfarin is enhanced by antibiotics.
Antibiotics (e.g. tetracyclines) may reduce the vitamin K-synthesising bacteria in the gut and so decrease the availability of vitamin K for the hepatic formation of the vitamin K dependent clotting factors: II, VII, IX and X, thus enhancing the anticoagulant effect of warfarin. Heparin acts at a large number of sites accelerating the neutralization of factors IXa, Xa, XIIa and promotes the inhibition of thrombin synthesis. The latency of the speed of onset of the anticoagulant effect of warfarin is dependent primarily on the rate of disappearance of the vitamin-K-dependent clotting factors that were preformed before commencing warfarin therapy. Vitamin K deficiency (not Vitamin A), impairs blood coagulation and therefore enhances the action of warfarin. Salicylates (such as aspirin) prolong prothrombin time by antagonizing the action of Vitamin K and inhibit platelet aggregation; these effects therefore enhance any warfarin anticoagulant action. |
Question 5 | |||||
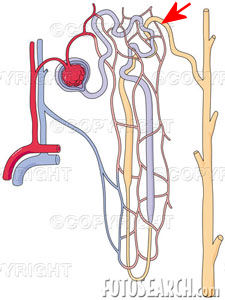 One of the following statements is true regarding the area of the renal nephron indicated (by the red arrow) on the above diagram: | |||||
| |||||
|
Answer: (e) Thiazides act here to inhibit active sodium reabsorption.
The portion of the nephron highlighted is the distal convoluted tubule. A summary of where various diuretics act on the nephron is shown below. 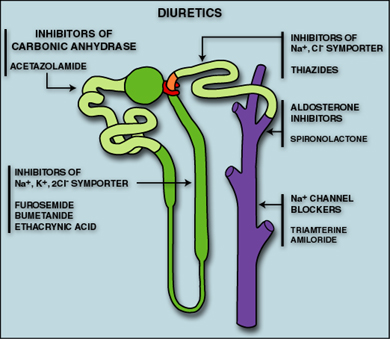 Thiazides act on the early portion of the distal convoluted tubule to inhibit active sodium reabsorption, they have no effect on the corticomedullary concentration gradient. Bumetanide and furosemide are loop diuretics and therefore act at the medullary segment of the ascending loop of Henle. Spironolactone is an aldosterone inhibitor and does act at the distal tubule though further along from the early segment of the distal tubule that thiazides act upon. Aldosterone causes urinary potassium loss (not reabsorption) hence the potential for spironolactone to cause hyperkalaemia. |