| Medical Finals contents: Welcome Finals advice Written exams Clinical revision X-Rays Mock final OSCE's |  |
Medical Finals contents: Monthly quiz PDA's Links Credits Your comments Who are we? |
Question 1 | |||||
|
A 55 year-old women is acutely short of breath 2 days following a left hemi-colectomy. A CXR showed a small left sided pleural effusion. The lungs were clear.
The consultant surgeon was concerned that his patient may have had a post-operative pulmonary embolus and requested a CT pulmonary angiogram (shown below). 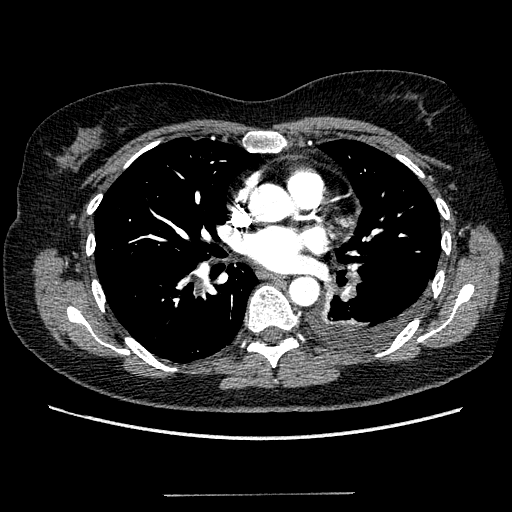 What do you think the cause of her shortness of breath is due to? | |||||
| |||||
Answer: (c) A pulmonary embolus
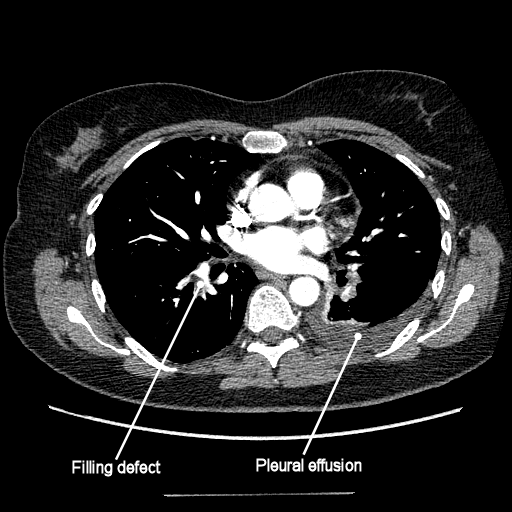 The clinical diagnosis of pulmonary embolus can be difficult. A D-dimer may be performed which if negative has a good negative predictive value, but is less useful if positive. Causes of a falsely raised d-dimer include: post operative status, malignancy and recent trauma. Although some centers still perform V-Q perfusion imaging for the diagnosis of PE it is fraught with difficulties not least in those with pre-existing chest disease. Computed tomography pulmonary angiography (CTPA) is now the imaging modality of choice. Conventional pulmonary angiography is reserved for special circumstances. CT imaging of the chest is performed with maximal contrast opacification of the pulmonary arteries (different from the arterial phase used for standard CT chest imaging). As the pulmonary arteries (and its segmental and sub-segmental arteries) are filled with contrast, any emboli within these structures will be highlighted as filling defects. Pulmonary emboli are seen as filling defects within the arteries – that is to say clot prevents contrast from filling this area. This CTPA demonstrates (see annotations) a large embolus within a segmental branch of the right lower lobe pulmonary artery. There is a small right sided pleural effusion (common post-op) but unlikely to be the cause of her sudden shortness of breath. |
Question 2 | |||||
|
An 18 year old girl presents to the emergency department extremely unwell. She is short of breath, cold and clammy to touch. She states she is very thirsty. The triage nurse reports to you that her blood glucose level is 21.2 mmol/l, and that she has ++++ ketones on urinalysis. Treatment is commenced.
What electrolyte should you be most concerned with monitoring over the next 24 hours? | |||||
| |||||
|
Answer: (b) Potassium
The patient has diabetic ketoacidosis as evidenced by:
The treatment regimen should comprise of insulin and intravenous fluids. Insulin acts to lower blood glucose levels, but also causes a fall in serum potassium. Potassium levels should be monitored frequently, since hypokalaemia can precipitate cardiac arrhythmias or cardiac arrest. Potassium should be carefully replaced in the intravenous fluids regime. |
Question 3 | |||||
| Which of the following signs are not associated with severe pulmonary hypertension? | |||||
| |||||
|
Answer: (d) Pan-systolic murmur loudest at the lower left sternal edge in expiration
Pulmonary hypertension can cause a variety of signs. The signs can be explained by remembering that this condition essentially makes it difficult for the blood to leave the right side of the heart. Thus, classical signs are (working your way from the heart backwards):
The murmur of tricuspid regurgitation is best heard at the lower left sternal edge, but since it is a murmur originating from the right side of the heart, it is louder in inspiration. Remember - left sided heart murmurs are loudest in expiration, and right sided murmurs loudest in inspiration. |
Question 4 | |||||
|
An ambulance is called to a pop concert, after a 14 year girl collapsed. Her friends state that she collapsed and had a few rhythmical jerks of her limbs. She was not injured, did not bite her tongue, but was incontinent of urine. When she regained consciousness she said that before blacking-out her vision faded and that her hearing became muffled.
What investigations are required? | |||||
| |||||
|
Answer: (d) None
This teenage girl has had a syncopal event and does not need to be investigated. The give-away clues include the circumstances – a pop concert, a crowded place, high emotion, standing up etc. She suffers a few jerks, which can occur in syncope due to decreased oxygen to the brain. These are usually brief and very subtle. These can appear misleading to the untrained observer, who may report them as seizure activity. If her bladder was full, then it is not uncommon to have incontinence, although not typical of syncopal episodes. The symptoms she described of altered vision and hearing alteration are classical of pre-syncope. To summarize the diagnosis is in the history. |
Question 5 | |||||
|
A 42 year old man presented to his GP with troublesome headaches mainly occurring at night. He describes them as excruciating, and during an attack his wife states that he becomes aggressive, noisy and has been known to kick furniture and walls. The headaches usually last about 60 minutes and occasionally his left eye becomes red and injected. It sometimes droops, making his wife think that he is having a stroke. He can sometimes have up to 6 attacks per night. Bad bouts occur every 3-4 months. He is well in between these episodes.
What is the diagnosis? | |||||
| |||||
|
Answer: (d) Cluster headache
This is a classical history for cluster headache. They tend to occur in middle aged men. They cluster. They typically last up to 180 minutes. They tend to occur at night and individuals tend to be restless during attacks. This is in contrast to migraine, when individuals classically take to their bed. There can be other autonomic symptoms of an injected eye and ptosis. |