| Medical Finals contents: Welcome Finals advice Written exams Clinical revision X-Rays Mock final OSCE's |  |
Medical Finals contents: Monthly quiz PDA's Links Credits Your comments Who are we? |
Question 1 | |||||
|
A 22 year old man had been out drinking after a victory for his local football team.
The following day whilst at work seated at his computer he lost consciousness and was told by his colleague that he fitted. It occurred without warning and lasted 2 minutes. He bit his tongue, was incontinent of urine and had a headache for the remainder of the day. A finger prick glucose measurement taken by paramedics measured 4.2 mmol/l. He had no similar previous episodes and has had none since. Clinical examination was normal. An EEG performed 1 month later was reported as normal. Based on this information, what is the most likely diagnosis? | |||||
| |||||
|
Answer: (c) Provoked seizure
This young man has most likely suffered a provoked seizure after a period of heavy drinking and sleep deprivation. Both of these stimuli lower any individualís seizure threshold. Certainly the event has all the features of a fit, including tongue biting and incontinence, with a post-ictal period. It is unlikely to be primary generalised epilepsy given the fact that his EEG trace was normal. |
Question 2 | |||||
|
The patient described in Question 1 above, is now concerned about driving.
What advice do you give him? | |||||
| |||||
|
Answer: (c) That he should inform the DVLA and stop driving for 12 months
Without doubt, driving is now a concern. Guidelines regarding this are laid out by the DVLA and are available on the web (http://www.dvla.gov.uk/medical.aspx). It is the patientís responsibility to inform the DVLA after such an event and the current guidelines state that you must be seizure free for 12 months before you can drive again. This stipulation includes provoked seizures caused by alcohol. The medical professional should inform the patient of the law regarding driving, but cannot enforce it. It is ultimately up to the patient to inform the licensing authority of any changes in their medical condition. |
Question 3 | |||||
|
A 56 year old Indian man presents to A&E after a seizure.
A CT scan is performed. His temperature is 37.7įC. His full blood count, CRP and chest x-ray are normal. Examination is unremarkable apart from a visual field defect. On exploring his history, the following day, he tells you that he had a renal tumour removed years ago, and that he recently had been home to India to visit relatives. His CT is shown below: 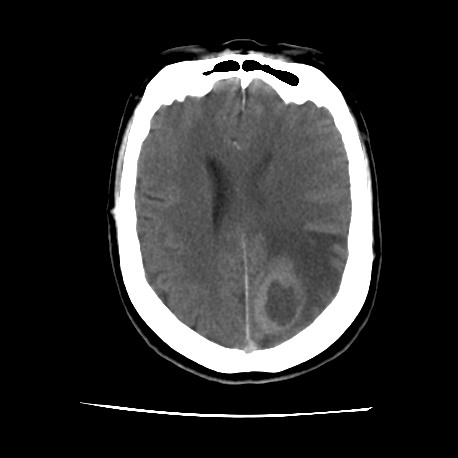 Which of the following is the most unlikely diagnosis? | |||||
| |||||
|
Answer: (e) Posterior circulation infarct
This CT scan demonstrates a ring enhancing lesion with surrounding oedema. All of the stems can potentially cause such an appearance, however an infarct would be most unlikely to do this. TB is unlikely here given the normal white cell count, CRP and chest x-ray, although it is an important differential given his racial origin and recent foreign travel. The normal blood parameters also make an abscess less likely, though not impossible. With his history of a previous tumour and the appearance on the scan, a primary or secondary deposit are certain possibilities. |
Question 4 | |||||
| For the patient in Question 3 above, which of the following would be the best diagnostic investigation? | |||||
| |||||
|
Answer: (d) Brain biopsy
In order to obtain a definitive diagnosis a tissue diagnosis is required. The best way of doing this is with a stereotactic CT-guided brain biopsy. |
Question 5 | |||||
|
A 74 year old man was admitted to hospital after he was found collapsed at the roadside.
Over the following hours he was noted to have a fluctuating level of consciousness. His blood alcohol level measured 389 mg/100ml (legal limit <80/100 ml). Here is his CT scan: 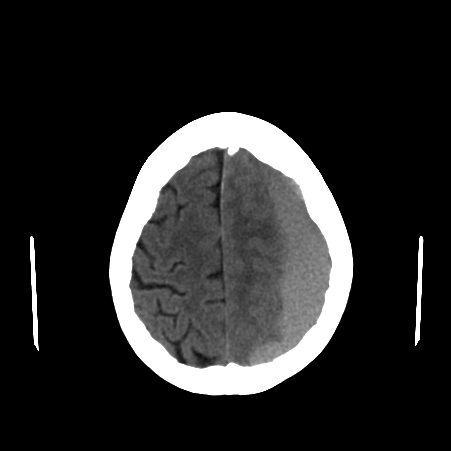 Based on the above information and the brain imaging what is the most likely diagnosis? | |||||
| |||||
|
Answer: (b) Subdural haemorrhage
This is a classical presentation of a subdural haemorrhage, as demonstrated by the concave density seen on the CT scan. Subdural haemorrhage occurs most commonly in the elderly and in alcoholics. The cause is typically trauma to the middle meningeal artery. |